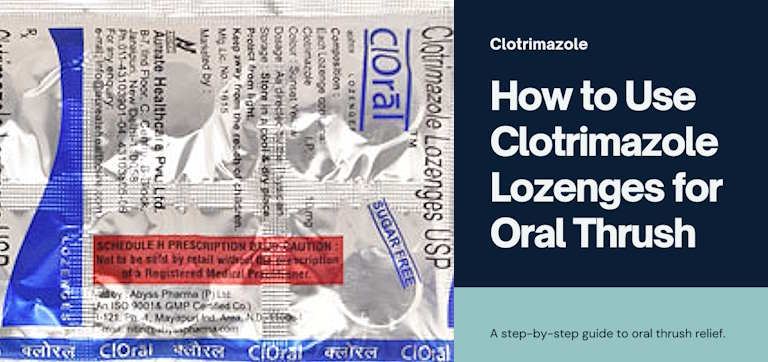
How to Use Clotrimazole Lozenges for Oral Thrush Relief
Table of Contents
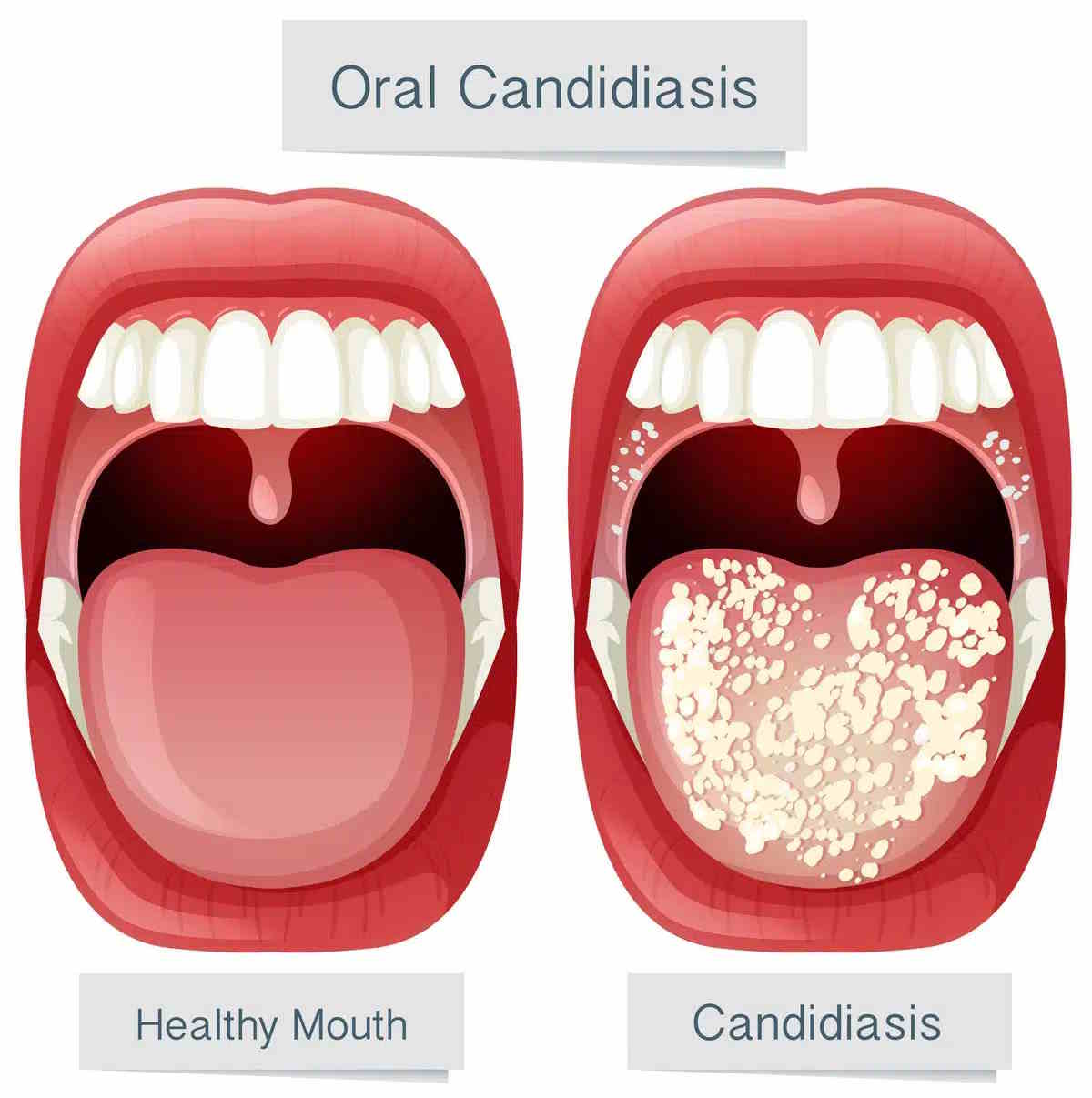
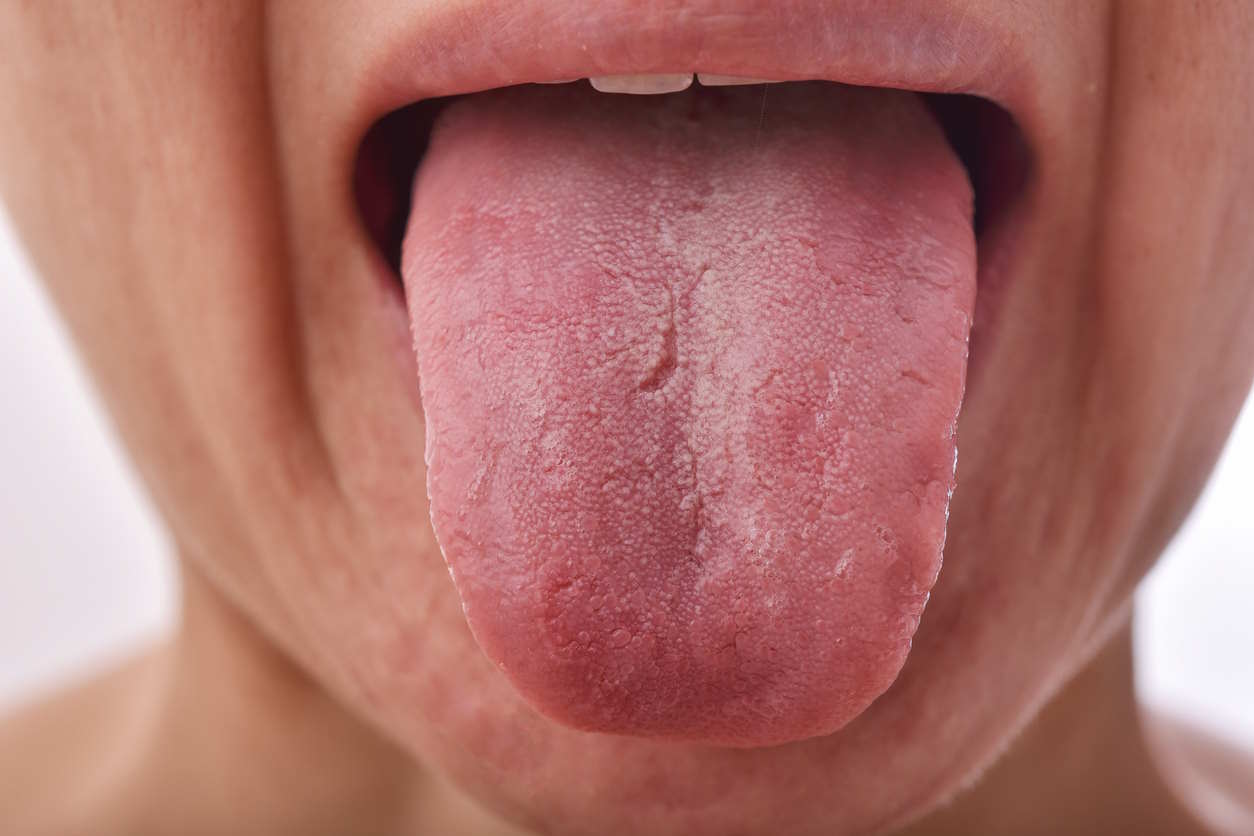
Oral thrush, which is a common fungal infection characterized by the overgrowth of Candida albicans fungus in the oral cavity, can be an uncomfortable and distressing condition for many people to endure. From difficulty in swallowing (dysphagia) to persistent discomfort, its symptoms can significantly impact one’s quality of life.
Fortunately, oral thrush relief is within reach with the effective use of antifungal agents such as clotrimazole lozenges and tablets. In this guide, we’ll explore clotrimazole’s effectiveness, application methods, and key considerations for managing oral thrush with clotrimazole 10mg lozenges.
What is Oral Trush?
Oral thrush, also known as oral candidiasis, is a fungal infection caused by Candida species, primarily Candida albicans.
Candida species are normal inhabitants of the oral cavity but can proliferate under favorable conditions, leading to colonization of oral mucosa. When there are factors disrupting the oral microbiome or the host’s immune system is weekend, these opportunistic fungi will grow significantly inside the oropharynx leading to the characteristic white patches and discomfort associated with oral thrush.
Individuals with weakened immune systems due to conditions such as HIV/AIDS, diabetes mellitus, or those undergoing chemotherapy or using corticosteroids are especially at increased risk of developing these types of fungal infections.
Treatment Options for Oral Thrush
Treatment options that are currently available for oral thrush include antifungal medications like nystatin, itraconazole, clotrimazole, or fluconazole, often administered as lozenges, mouth rinses, or oral tablets.
Additionally, antiseptic mouthwashes containing chlorhexidine can help reduce fungal populations. Topical antifungal creams may be prescribed as well.
What is Clotrimazole?
Clotrimazole is a broad-spectrum antifungal medication that belongs to the class of antifungal medications known as azoles that treat various fungal infections.
It exerts its antifungal activity by inhibiting the synthesis of ergosterol, an essential component of the fungal cell membrane. Ergosterol is vital for maintaining membrane integrity and function in fungi, hence, by blocking ergosterol synthesis, clotrimazole can disrupt the fungal cell membrane, causing leakage of cellular contents and ultimately leading to cell death.
It is available in different forms such as creams, lotions, powders, and vaginal suppositories. Here’s a breakdown of its indications and contraindications:
Indications:
- Oral Thrush: Clotrimazole may be prescribed in oral form or lozenges to treat oral thrush (oral candidiasis), a fungal infection of the mouth and throat.
- Fungal Infections: Clotrimazole is primarily used to treat fungal infections of the skin, such as athlete’s foot (tinea pedis), jock itch (tinea cruris), ringworm (tinea corporis), and yeast infections (candidiasis).
- Vaginal Yeast Infections: It is also commonly used in the form of vaginal suppositories or creams to treat vaginal yeast infections (vulvovaginal candidiasis).
Contraindications:
- Allergy: Individuals with a known allergy to clotrimazole or any of its components should avoid using it.
- Pregnancy: While clotrimazole is generally considered safe during pregnancy, it’s advisable to consult a healthcare provider before using it, especially during the first trimester.
- Breastfeeding: It is generally safe to use clotrimazole while breastfeeding, but consulting a healthcare provider is recommended to ensure its safety for both the mother and the infant.
- Open Wounds: Clotrimazole should not be applied to open wounds or areas of broken skin as it may cause irritation or adverse reactions.
- Children: While clotrimazole is often used in children, specific formulations and dosages may be necessary, and it’s important to follow the guidance of a healthcare provider
Clotrimazole Tablets for Oral Thrush
The utilization of clotrimazole tablets for oral thrush brings forth a straightforward approach to treatment. Administered orally, these tablets deliver the antifungal agent directly to the affected area, swiftly alleviating symptoms and restoring oral health.
-

Candid® Clotrimazole Cream / Powder
Clotrimazole 1% / 2%, Beclometasone, Ofloxacin, Ornidazole, Terbinafine, Clobetasol, Miconazole, Neomycin
Size: 20g / 0.7oz
Brand name: Canesten, Lotrimin, Gyne-Lotrimin, Diprolene, Luxiq, Floxin, MetroGel, Lamisil AT, Temovate, Dermovate, Clobex, Olux, Monistat, Micatin, Neo-Synalar
From USD $18.00 Select options -
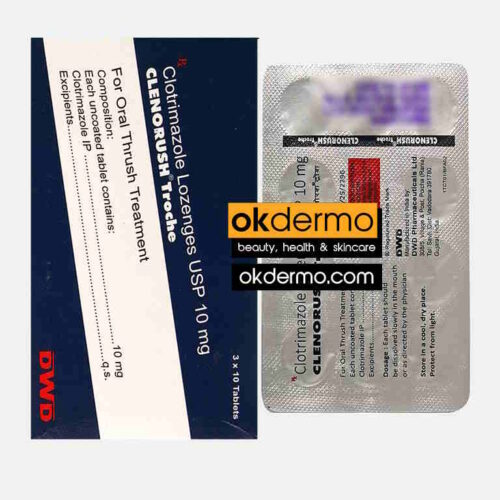
Clenorush Troche® Clotrimazole Lozenges
Clotrimazole 10mg
Size: 30 Lozenges
Brand name: Canesten, Clotrimaderm, Desenex, Myclo-Derm, Neo-Zol, Clotrim, Antifungal, Cruex, Lotrimin, Mycelex
USD $38.00 Add to cart
Clotrimazole 10mg lozenges
While both clotrimazole tablets and lozenges contain the same active ingredient and are used to treat fungal infections, they are formulated differently to target specific areas of the body and are used accordingly. Tablets are typically for vaginal or oral use, while lozenges are specifically for oral use.
Clotrimazole 10mg lozenges particularly stand as a cornerstone in the treatment of oral thrush as they directly tackle the fungal overgrowth in the oropharynx that is responsible for this condition. These lozenges offer convenience and effectiveness in combating the discomfort caused by oral thrush.
Efficacy
Clotrimazole lozenges have demonstrated efficacy in the treatment of oral thrush, with clinical studies showing significant improvement in symptoms and clearance of fungal infection following treatment. The slow dissolution of the lozenge allows for prolonged exposure of the oral mucosa to clotrimazole, enhancing its antifungal effects.
How to use clotrimazole lozenges for oral thrush
For the treatment of oral thrush, mycelex lozenges (clotrimazole) are typically administered orally. To use clotrimazole lozenges for oral thrush, gently place one in your mouth and let it dissolve slowly without chewing. Avoid eating or drinking for about 30 minutes after use and monitor for any side effects and contact your healthcare provider if needed.
The recommended dosage is one 10mg lozenge dissolved slowly in the mouth five times daily for 14 days. When used for initial HIV 1 treatment, the duration is typically 7-14 days.
It’s important for patients to follow the prescribed regimen consistently to ensure effective eradication of the fungal infection.

Clotrimazole Lozenge Side Effects
While generally well-tolerated, like all medications, clotrimazole lozenges can potentially cause side effects. It is essential for healthcare providers and patients to be aware of these side effects to ensure safe and effective treatment. Here is a comprehensive overview of the possible side effects associated with clotrimazole lozenges:
Common Side Effects:
- Oral Irritation: Patients may experience mild irritation or burning sensation in the mouth upon using clotrimazole lozenges. This usually resolves on its own and does not require discontinuation of treatment.
- Nausea: Some individuals may experience mild nausea as a side effect of clotrimazole lozenges. This side effect is usually temporary and resolves without intervention.
- Vomiting: In rare cases, clotrimazole lozenges may cause vomiting, particularly if the medication is accidentally swallowed instead of being allowed to dissolve slowly in the mouth. Patients should be instructed on the proper administration technique to minimize this risk.
- Change in Taste: A temporary alteration in taste perception, often described as a metallic or bitter taste, may occur with the use of clotrimazole lozenges. This side effect typically resolves once treatment is completed.
Rare Side Effects:
- Allergic Reactions: Although uncommon, some individuals may experience allergic reactions to clotrimazole lozenges. Symptoms of an allergic reaction may include rash, itching, swelling of the face or throat, severe dizziness, or difficulty breathing. Patients should seek immediate medical attention if they experience any of these symptoms.
- Liver Toxicity: In rare cases, clotrimazole lozenges may cause liver toxicity, characterized by symptoms such as jaundice (yellowing of the skin or eyes), dark urine, abdominal pain, or unusual fatigue. Patients should discontinue the medication and consult their healthcare provider if they experience any signs of liver toxicity.
- Adverse Drug Interactions: Clotrimazole lozenges may interact with certain medications, including anticoagulants (blood thinners) such as warfarin, leading to an increased risk of bleeding. Patients should inform their healthcare provider about all medications they are taking before starting treatment with clotrimazole lozenges.
Oral thrush prevention
To prevent oral thrush, it’s essential to understand its underlying causes and risk factors. Oral thrush, also known as oral candidiasis, is typically caused by an overgrowth of the fungus Candida albicans in the mouth. Here are some important mechanisms and strategies for prevention:
- Maintain Good Oral Hygiene: Proper oral hygiene is crucial in preventing oral thrush. Encourage your patients to brush their teeth at least twice a day and floss regularly. Additionally, using an antimicrobial mouthwash can help reduce the risk of fungal overgrowth.
- Limit Sugar and Yeast Intake: Candida albicans thrives on sugar and yeast, so reducing the consumption of sugary and yeasty foods can help prevent oral thrush. Advise patients to limit their intake of sweets, sugary beverages, and foods containing yeast.
- Manage Underlying Conditions: Certain medical conditions and medications can increase the risk of oral thrush. For example, immunocompromised individuals, such as those with HIV/AIDS or undergoing chemotherapy, are more susceptible to fungal infections. Proper management of underlying conditions and medications can help reduce the risk.
- Avoid Smoking and Alcohol: Smoking and excessive alcohol consumption can weaken the immune system and disrupt the balance of microorganisms in the mouth, increasing the risk of oral thrush. Encourage patients to quit smoking and limit alcohol intake.
- Use Probiotics: Probiotics are beneficial bacteria that can help maintain a healthy balance of microorganisms in the mouth and gut. Consuming probiotic-rich foods or supplements may help prevent oral thrush by inhibiting the growth of Candida albicans.
Conclusion
In conclusion, clotrimazole lozenges, particularly in the form of 10mg tablets, serve as a cornerstone in the management of oral thrush. By adhering to optimal dosage guidelines and being vigilant of potential side effects, individuals can harness the full potential of clotrimazole lozenges for effective relief. Whether utilizing clotrimazole tablets or Mycelex lozenges, the path to oral health is within reach with these powerful antifungal agents.
FAQs
-
How long do clotrimazole lozenges take to work?
Clotrimazole lozenges typically start to work within a few days of regular use. However, noticeable improvement may vary depending on the severity of the condition and individual response.
-
How long does it take for oral thrush to go away with clotrimazole?
Oral thrush treated with clotrimazole usually shows improvement within a week of consistent use. However, complete resolution may take up to two weeks. It’s essential to follow the prescribed treatment duration for the best results.
-
Do you swallow clotrimazole troche?
No, clotrimazole troches are meant to be slowly dissolved in the mouth, not swallowed whole. Follow the specific instructions provided by your healthcare provider or pharmacist for the proper administration of clotrimazole troches.
-
Is clotrimazole good for oral thrush?
Yes, clotrimazole is an antifungal medication commonly used to treat oral candidiasis. It works by targeting the fungal infection responsible for oral thrush, helping to alleviate symptoms and promote healing when used as directed.
References
- Pappas PG, Kauffman CA, Andes DR, et al. Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;62(4):e1-e50. doi:10.1093/cid/civ933
- Vazquez JA, Patton LL, Epstein JB, et al. Randomized, Comparative, Double-blind, Double-dummy, Multicenter Trial of Miconazole Buccal Tablet and Clotrimazole Troches for the Treatment of Oropharyngeal Candidiasis: Study of Miconazole Buccal Tablet for Oropharyngeal Candidiasis. Clin Infect Dis. 2007;44(8):1051-1059. doi:10.1086/512681
- Jepsen K, Klausch T, Wolff A, Perner S, Grosse U, Gründer U. Miconazole Buccal Tablets in the Treatment of Candida-Associated Denture Stomatitis: A Comparative Study. Clin Oral Investig. 2013;17(3):815-821. doi:10.1007/s00784-012-0757-2
- Dangi YS, Soni ML, Namdeo KP, Jain SK. A Review on the Strategies for Oral Delivery of Clotrimazole: A Potent Antifungal Agent. Pharmaceutica Analytica Acta. 2013;4(3):1-8. doi:10.4172/2153-2435.1000223
- Villar CC, Kashleva H, Nobile CJ, Mitchell AP, Dongari-Bagtzoglou A. Mucosal Tissue Invasion by Candida albicans Is Associated with E-Cadherin Degradation, Mediated by Transcription Factor Rim101p and Protease Sap5p. Infect Immun. 2007;75(5):2126-2135. doi:10.1128/iai.01484-06
Post by:
Dr.Marcella Jiovanni
Health and Beauty Expert
“Marcella Jiovanni actively promotes the importance of maintaining healthy skin, she envisions the future of dermatology as moving away from pure medical, pharmacological dermatology and flowing more toward a holistic approach to wellness and skincare.”